The Community-based Health System Model briefs identify and discuss critical health system inputs and processes that have contributed to the implementation and expansion of community-based service delivery in different countries. Countries were selected for their geographic diversity, type of service delivery model, and programmatic scale-up. This brief reviews Nepal's community health model to inform future policy, program design, and implementation in other countries. Read briefs on Malawi | Senegal

Health Situation in Nepal
Nepal has made impressive progress in reducing infant, child, and maternal mortality since it began providing community-based service delivery 20 years ago.1 Since 1990, the maternal mortality ratio (MMR) has declined by more than two-thirds, from 850 deaths per 100,000 live births in 1990 to 190 in 2011.2 Nepal is one of a few countries in South Asia to achieve the Millennium Development Goal (MDG) 4 target to reduce child mortality by two-thirds and was close to achieving the MDG 5 target to reduce maternal mortality by 75 percent. These achievements can be at least partially attributed to the political will of the Government of Nepal (GON) and the continually evolving community-based health services provided by the three cadres of community-level service providers (CLSPs): female community health volunteers (FCHVs), auxiliary nurse midwives (ANWs) and auxiliary health workers (AHWs).2 Until recently, two other cadres—village health workers (VHWs) and maternal and child health workers (MCHWs)—operated in Nepal, but were upgraded to AHWs and ANMs. See Table 1 for Nepal's health statistics.
Table 1. Current Health Statistics in Nepala
| Total population | 26.6 M |
| Rural populationb | 82% |
| Total fertility rate | 2.6 |
| Contraceptive prevalence rate (modern methods) | 43.2% |
| Maternal mortality ratio (per 100,000 live births)c | 190 |
| Neonatal mortality rate (per 1,000 live births) | 33 |
| Infant mortality rate (per 1,000 live births) | 46 |
| Under-five mortality rate (per 1,000 live births) | 54 |
| Percentage of births delivered by a skilled provider | 36.0% |
| Percentage of children moderately or severely stunted | 40.5% |
| Percentage of households with an improved source of drinking water | 88.9% |
| Percentage of women reporting distance to a health facility as a problem in accessing health care | 46.6% |
| Adult HIV prevalenced | 0.2% |
| Total expenditure on health per capita (current US$)e | $39 |
a Data is from Nepal Demographic and Health Survey, 20114, unless otherwise noted.
b United Nations, Department of Economic and Social Affairs, Population Division (2015). World Urbanization Prospects: The 2014 Revision, (ST/ESA/SER.A/366).
c World Health Organization, UNICEF, UNFPA, The World Bank & the United Nations Population Division. 2014.Trends in maternal mortality: 1990 to 2013. Geneva, Switzerland: WHO.
d UNAIDS. 2014. "HIV and AIDS estimates."
e World Bank DataBank. 2010-2014. "Health expenditure per capita (current US$)."
More than 90 percent of Nepalis receive their health services, including family planning, at the community level.
Despite this progress, neonatal and infant mortality continue to be high (33 and 46 deaths per 1,000 live births, respectively). Further, preventable infant- and child-specific diseases, such as diarrheal diseases and respiratory infections, are among the top 10 leading causes of death in Nepal, irrespective of age group.3 Overall, mortality rates are higher in rural areas compared with urban areas, particularly in the mountainous regions, due to limited health infrastructure and challenging terrain.4 Yet, over the course of 15 years, rural areas in Nepal have experienced more drastic reductions in under-5 mortality, with deaths dropping by more than 50 percent between 1996 and 2011,4,6,7,8 notably narrowing the urban/rural gap, as depicted in Figure 1.
Figure 1. Under-five Mortality by Urban and Rural Areas in Nepal, 1996-2011*
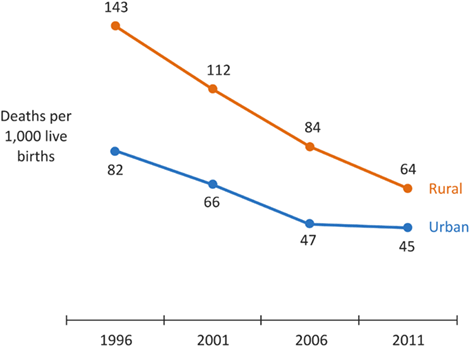
* Data are from Nepal Demographic and Health Survey, 1996, 2001, 2006 and 2011
More than 90 percent of Nepalis receive health services, including family planning (FP), at the community level.5 Data show that from 1996 to 2011, the use of modern FP methods has greatly increased in rural areas, as shown in Figure 2. Further, contraceptive prevalence rate (CPR) has increased most among women in the poorest wealth quintile, from 30.3 percent in 2006i,6 to 35.6 percent in 2011.4
Figure 2. Current Use of Modern Methods of Family Planning in Nepal, 1996-2011*

* Data are from Nepal Demographic and Health Survey, 1996, 2001, 2006 and 2011
Nepal's Health System Structure: Community Health Workers Are Essential to Reaching the Underserved
Nepal's public health system is decentralized and guided by policies on health service delivery, human resources, information systems, and the cost of services for patients.
The country has a mixed health service delivery system, comprised of the public sector, private for-profit sector, and nongovernmental organizations (NGOs). The Ministry of Health (MOH) serves rural, underserved populations; private providers, including NGOs and faith-based organizations (FBOs), predominantly serve urban populations.9,10
Health policy is developed, standardized, and governed at the central level by the MOH. Services are delivered at the five lower levels, from the regional to the community (see Figure 3). The community level includes two political levels, the village development committee (VDC) and the ward. Services at the VDC are delivered through health posts (HPs), which are staffed by AHWs and ANMs, paid health workers who are employed by the MOH. At the ward level, services are provided in the community by FCHVs.ii This cadre of service providers delivers a basic package of essential maternal and child health (MCH) services including FP, antenatal care, immunization, and nutrition. Additionally, the three cadres of CLSPs (FCHVs, AHWs, and ANMs) deliver outreach services for immunization and primary health care (PHC) in the community to extend the full range of services available at the HPs. Each level of the public health system is linked by a formal, coordinated referral system.11
Figure 3. Nepal's Public Health System
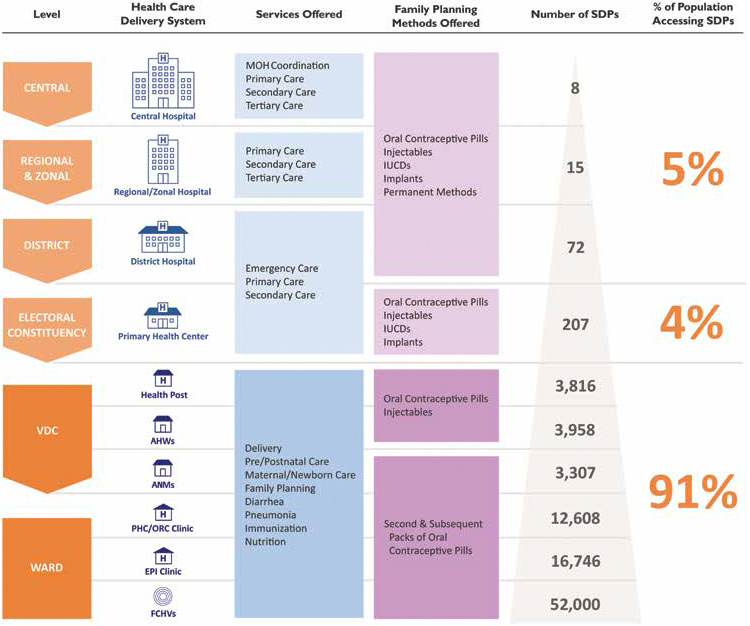
Nepal's health policy environment and health service delivery system have evolved over the past 25 years. The health system has moved from centralized to decentralized management, leading to more management structures at the district and VDC levels. This decentralized organization, as well as the gradual addition of health services starting with provision of basic FP services to delivery of child health medicines and life-saving maternal health services, has led to availability of a comprehensive package of MCH services at the community level.10
These changes have contributed to improvements in the uptake of health services and MCH outcomes. For instance, the CPR for modern methods rose from 26 percent in 19968 to 43.2 percent in 2011,4 with over 50 percent of all oral contraceptives being provided by FCHVs.5 Similarly, vitamin A supplementation for children 6-59 months, a commodity predominantly distributed by FCHVs and CLSPs, increased from 32.3 percent in 19968 to 90.4 percent in 2011.4
Key Community Health System Inputs: Policy to Service Delivery
There are many approaches to designing and implementing community health service delivery systems to achieve universal health care, and in particular to reach the most vulnerable populations. From policy to service delivery, the critical elements to scaling up Nepal's community health program have been captured in Table 2.
Table 2. Key Inputs in Nepal's Community Health Program11
| INPUT | NEPAL'S COMMUNITY HEALTH PROGRAM |
|---|---|
| Supportive policy | There are three policies for community-based health service delivery: 1. FCHV Strategy, 2010 2. Community Based Integrated Management of Newborn and Childhood Illness Package Guidelines, 2014 3. Community Based Neonatal Care Package Guidelines, 2007 |
| FCHV Selection | Women 24-45 years old, with 3 or fewer children preferred; selected by community groups. |
| Supervision and management | Supervised by higher-level cadres of CLSPs (e.g., nurse midwives) who report and make referrals to higher-level facilities. |
| Commodities and materials | Provided with a basic package of social and behavioral change communication (SBCC) job aids; reporting forms; health commodities ordered through health logistics management system including ORS, zinc, Vitamin A, oral contraceptive pills, male condoms, albendazole, chlorhexidine, iron tablets, and misoprostol (currently in select districts); and CLSP identification card after training. |
| Training | FCHVs receive an 18-day basic training with refresher training every five years, undergo shorter annual training updates, and attend monthly meeting and other program related training such as misoprostol. |
| Incentives | FCHVs receive a combination of financial and non-financial incentives provided by the MOH and VDCs; AHWs and ANMs are formally paid by the MOH. |
| Referrals | FCHVs use a paper-based form to refer clients to AHWs, ANMs, or a HP, depending upon services needed. |
| Health promotion | FCHVs conduct monthly meetings with health mothers' groups. |
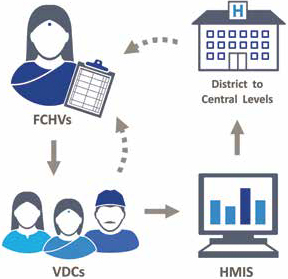
| Monitoring and reporting | Paper-based data collection is incorporated into a national health management information system (HMIS) by CLSP supervisors and used for national-level program decision making and community-level supervision. |
| Scope of practice | Clear job descriptions and associated trainings exist for each CLSP role: FCHVs distribute health commodities for childhood illnesses, FP, antenatal care, and maternal health and conduct health promotion and skill building activities in these topical areas. AHWs supervise FCHVs and distribute first aid commodities, immunizations, misoprostol and chlorhexidine (CHX), ORS, zinc, cotrimaxozole, oral contraceptive pills, male condoms, and injectable contraceptives, and provide information and education for FP, child and maternal health, nutrition, respiratory infections, and antenatal and postnatal care. ANMs have the same SOP as AHWs but also provide services and education related to ante-natal and postnatal care. |
While these inputs are important to a well-functioning community service delivery system, some countries implement certain areas more effectively than others. Nepal's community health system delivers a comprehensive package of essential MCH services nationwide, which is probably possible because of several factors:
- Implementation of clear scopes of practice for FCHVs.
- A health logistics system that delivers essential medicines to the hardest to reach and serves (last mile) communities.
- A strong information management system to collect service delivery indicators at the community level.
- A varied, community-driven incentive package to motivate volunteer workers.
These strong community health service delivery inputs have led to a nationwide program with health outcomes that have improved over time and are described in further detail below.
Key Strategies for Strengthening and Scaling Up Nepal's Community Health Program
Key Points:
- Prior to the formalization of the community-based system in the 1980s, service delivery was directed at the regional level. Service guidelines were not clear and training was not standardized. Currently, SOPs are directed from the central level, ensuring standard approaches to community-level health care across the country.
- Nepal's community health system has been evolving for over 20 years. Allowing time to expand the scope and role of FCHVs allows policymakers and program managers to understand and mitigate barriers to service delivery, training, reporting, and logistics before more responsibilities are added.
1. Expanding FCHV scopes of practice over time
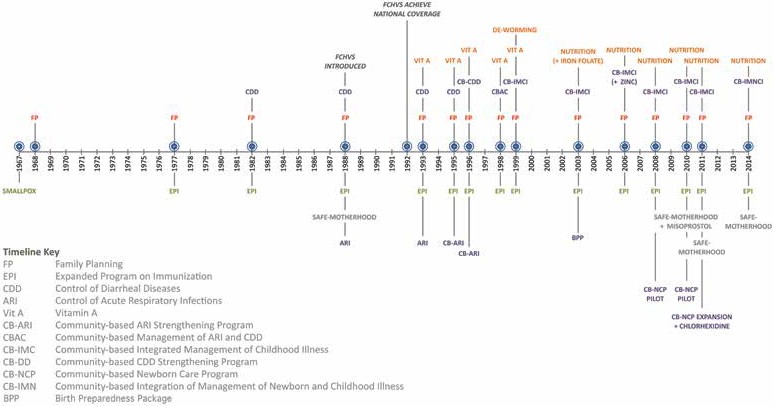
In 1967, a national smallpox eradication program that had started as a pilot project in three districts was launched. One year later, the delivery of basic FP services was added to the scope of community health providers, who were largely supported by NGOs. By 1977, Nepal declared eradication of smallpox, and initiated a public sector Expanded Program on Immunization (EPI) using the same community platforms established through the smallpox program. The public sector community health system was formalized in 1988, starting with the selection and training of FCHVs. The initial scope of practice (SOP) included provision of oral contraceptive pills, male condoms, FP information, education, and communication; counseling on maternal health and antenatal care; and promotion of immunization services. FCHVs provided this basic package for four years while the program was scaled up from an initial 27 districts to all 75.12
Next, SOPs were expanded to include messaging about diarrhea prevention, provision of home treatment using oral rehydration salt (ORS) packets, and distribution of vitamin A. The MOH continued expanding the role of FCHVs in 1995 through a four-district pilot program that trained them to assess sick children for pneumonia, treat simple cases of pneumonia, refer more seriously ill children, and counsel mothers for all cases. Additional duties were added in 1999, 2003, 2006, 2008, 2010, and 2011 (see Figure 4).12 At present, the FCHV SOP includes delivery of comprehensive MCH services at the community level.11
Figure 4: Nepal's cHMIS Data Flow
Each service added to the FCHV SOP was accompanied by distinct and service-specific training curricula, materials, and job aids. FCHVs receive training at various skill levels to offer each new service to their communities.12
A national survey of FCHVs conducted in 2006 highlighted that a vast majority of FCHVs reported delivering the full range of services listed in their SOPs. For example, 99 percent of FCHVs reported that they provided counseling to pregnant women, 91 percent referred women for injectable contraceptives, and 82 percent examined children with symptoms of acute respiratory infections in the past month.13 FCHVs explained that some services, such as oral contraceptives and ORS, had lower-than-reported provision rates because of higher demand for long-acting contraceptive methods and frequent ORS stockouts, in addition to other issues.
2. Ensuring commodity availability through a demand-driven ordering system from the district to the community
In 1994, the GON created a central Logistics Management Division (LMD) responsible for improving the supply of essential medicines in the country. Over time, the LMD expanded training, strengthened logistics information reporting, and transformed the system into a demand-driven pull system.
Key Point:
FCHVs order their stock based on the demand of their clients rather than waiting for the commodities to be "pushed" to them. Logistics system improvements, coupled with the increased availability of commodities nationwide, increase access to essential medicines at the community level.
These improvements to the logistics system increased access to health commodities at the community level. The GON developed a logistics campaign to train all health workers across the health system. In 2006, AHWs and ANMs—then known as MCHWs and VHWs—began ordering health commodities for themselves and the FCHVs. Commodities were "pushed" from the sub health post level to FCHVs.15 In 2011, the pull
system expanded to the FCHV level.15 Each FCHV is provided with 45 days of stock to ensure adequate monitoring and supervision of commodity distribution.
The results of the latest FCHV survey conducted in 2014 show that stockouts of ORS have decreased. In 2014, 75 percent of FCHVs were equipped with ORS, compared with only 49 percent in 2006.13,16 While the country has made great strides in improving its logistics system, when stockouts occur they are more likely to happen at the community level than any other level.5
3. Monitoring routine health information and program effectiveness through an integrated cHMIS
Key Points:
- During early implementation of the community-based service package, there was no clear process for incorporating the service delivery data collected by FCHVs into the national HMIS, since the electronic reporting system stopped at the HP level. The expansion of the electronic reporting system to the community level increased the reporting rates of CLSPs.14,15
- Integrating community-level data into an electronic system eases data collection and reporting, particularly for less-skilled providers and improves completion of data collection and reporting rates.
Nepal utilizes a community health management information system (cHMIS) to assess the performance and effectiveness of community-level services. The cHMIS incorporates community-level data gathered by FCHVs through monthly delivery data collection forms that are then submitted to their AHW or ANM supervisors (see figure 4). While higher levels of the health system report a myriad of indicators through more than 40 registers, data collection forms at the community level are purposely integrated so less-skilled providers can complete them more easily. The supervisor then compiles the data into the HMIS, along with additional service delivery data from the HP, and then submits the information to the central level through standard reports that can be used in program monitoring.11
The implementation of an electronic cHMIS has improved community-level data reporting. Currently, around 97 percent of FCHVs17 and, as of 2012, 93 percent of VHWs and MCHWs18—now known as AHWs and ANMs—have recorded data into the cHMIS. These data are also used to inform the AHWs and ANMs supervision of FCHV performance in a relatively expedient fashion.
4. Provide a variety of incentives to keep volunteer CLSPs motivated
FCHV attrition is impressively low in Nepal, especially for a volunteer program. Annually, 4 percent of FCHVs leave their posts; in 2014, FCHVs had an average of 13.9 years of experience, with 46 percent of FCHVs having served for 16 years or more.16 The MOH uses an array of incentives to motivate FCHVs.13 These incentives provide direct and indirect benefits that contribute to a supportive environment and recognize the importance of FCHV's work.
Key Point:
According to the 2014 FCHV National Survey, FCHVs identified community appreciation as a factor that affected their motivation to help others.16 While many other countries have volunteers with similar direct incentives, Nepal's program stands out through the large-scale enabling environment created for FCHVs through motivators aimed at promoting and building FCHV recognition in the country. While there is community recognition in other countries, Nepal's approach is promulgated through mass media that reaches a larger population.13
Direct Benefits:
- Daily allowances of about US$4 are provided to FCHVs when they attend mass immunization days, trainings, and meetings.13
- A dress allowance (blue saris designed with the FCHV logo accompanied by an official name badge) gives FCHVs recognition in the community.
- Cash incentives are not universal but are provided by some VDCs. Of the 36 percent of FCHVs who reported receiving any incentives other than a dress allowance in 2014, 79 percent reported receiving cash.16
- Cash loans are offered through the FCHV Fund, a financial mechanism that gives access to a savings account managed at the VDC level. District- level governments contribute an initial $600 and provide annual contributions of $120 to a fixed bank account. FCHVs are able to withdraw funds from the savings for activities that support their performance.19 In 2014, an impressive 97 percent of FCHVs reported having an Endowment Fund in their VDC, and 60 percent reported having drawn on the fund in the last year.16
Indirect Benefits:13
- National FCHV Day is celebrated annually on December 5.
- A television drama featuring famous actors highlights FCHVs and their commitment to their work, creating a sense of celebrity status for FCHVs among community members.20
Lessons for Other Countries
Nepal's community health system continues to evolve to meet the growing health demands of its people. It has slowly expanded to include a comprehensive package of MCH services delivered by CLSPs. It is likely that key community health system inputs highlighted in this brief played a critical role in improving health outcomes, including MDGs 4 and 5, for underserved and vulnerable populations in the country. Lessons from Nepal's experience may be helpful for other countries that want to expand and/or implement their own community-based program. These include:
- Developing a community program on a nationwide scale is a gradual process. Nepal initiated its community program in 1967 through NGO engagement and slowly expanded the FCHV SOP. With each additional service, a training package was developed and systematically rolled out. The Government continues to adapt and change the scope of the FCHV program.
- Government commitment and stewardship to set policy and guide harmonization of community-level service provision are critical. Policymaking, supported by clear and comprehensive guidelines regarding the roles and responsibilities for CLSPs and their supervisors, helps set the agenda for training requirements, monitoring and reporting, information systems, and links between the community and the health facility.
- A "demand driven" pull ordering system allows CLSPs to obtain and manage their own stock, limit stockouts at the community level, and improve reporting rates. However, the stock of medicines carried by CLSPs should be for a time-bound period, such as one month. This forces CLSPs to go to a health facility for restocking and provides an opportunity for supervision to ensure appropriate distribution and service delivery, as well as reporting. A related important point is that governments should ensure a consistent supply of commodities to reduce stockouts, ensure health service delivery at the community level, and reinforce trust in the public health system overall.
- Utilize integrated data collection forms to streamline reporting processes and time spent on data collection, particularly for less skilled CLSPs. In Nepal, incorporating these community-level forms into the national HMIS has improved reporting rates and made the health needs of the community more visible. It may be important to consider the usability for CLSPs and the needs of national-level decision makers when designing a cHMIS.
- Motivate community health volunteers through a variety of local mechanisms that can be harmonized at the national level. Certain incentives should be determined by the community, tailored to its context. At the same time, national efforts such as mass media campaigns, uniforms, and badges have gone a long way to making FCHVs feel recognized and indispensable in Nepal.
Figure 5. Timeline of Nepal's Community Health Program
Reference List
i 2006 was the first year that the Demographic and Health Survey (DHS) provided data by wealth quintile.
ii A full list of the CLSP roles and responsibilities can be found in the Nepal Country Profile in the APC Community Health Systems Catalog.
1 Ministry of Health and Population (MOHP) [Nepal], New ERA, and ICF International Inc. 2012. Nepal Demographic and Health Survey 2011. Kathmandu, Nepal: Ministry of Health and Population, New ERA, and ICF International, Calverton, Maryland.
2 Government of Nepal National Planning Commission, United Nations Country Team of Nepal. 2013. ![]() Nepal Millennium Development Goals Progress Report 2013. Kathmandu, Nepal: Government of Nepal National Planning Commission (Accessed July 2014).
Nepal Millennium Development Goals Progress Report 2013. Kathmandu, Nepal: Government of Nepal National Planning Commission (Accessed July 2014).
3 Institute for Health Metrics and Evaluation. 2010. ![]() Global Burden of Disease Profile: Nepal. Seattle, WA: Institute for Health Metrics and Evaluation (Accessed September 2014)
Global Burden of Disease Profile: Nepal. Seattle, WA: Institute for Health Metrics and Evaluation (Accessed September 2014)
4 Ministry of Health and Population (MOHP) [Nepal], New ERA, and ICF International Inc. 2012. Nepal Demographic and Health Survey 2011. Kathmandu, Nepal: Ministry of Health and Population, New ERA, and ICF International, Calverton, Maryland.
5 Government of Nepal, Ministry of Health, Department of Health Services Annual Report 2012-2013. Kathmandu, Nepal: Department of Human Services.
6 Ministry of Health and Population (MOHP) [Nepal], New ERA, and Macro International Inc. 2007. Nepal Demographic and Health Survey 2006. Kathmandu, Nepal: Ministry of Health and Population, New ERA, and Macro International Inc.
7 Ministry of Health [Nepal], New ERA, and ORC Macro. 2002. Nepal Demographic and Health Survey 2001. Calverton, Maryland, USA: Family Health Division, Ministry of Health; New ERA; and ORC Macro.
8 Ministry of Health and Population (MOHP) [Nepal], New ERA, and ICF International Inc. 1997. Nepal Demographic and Health Survey 1996. Kathmandu, Nepal: Ministry of Health and Population, New ERA, and ICF International, Calverton, Maryland.
9 RTI International, 2010. ![]() Overview of Public-Private Mix in Health Care Service Delivery in Nepal. Research Triangle Park, NC, USA (Accessed July 2014).
Overview of Public-Private Mix in Health Care Service Delivery in Nepal. Research Triangle Park, NC, USA (Accessed July 2014).
10 Government of Nepal, Ministry of Health and Population. 2012. Human Resources for Health Strategic Plan 2011-2015 Draft. Kathmandu, Nepal.
11 Advancing Partners & Communities. 2014. Country Profile: Nepal Community Health Programs. Arlington, VA: Advancing Partners & Communities.
12 Houston R, Acharya B, Poudel D, Pradhan S, Singh S, Manandhar M, Pokharel RK, Shrestha PR. 2012. "Early Initiation of Community-based Programmes in Nepal: A Historic Reflection,"Journal of Nepal Health Research Council: 10 (21) 82-27.
13 New Era. 2007. ![]() An Analytical Report on National Survey of Female Community Health Volunteers. Kathmandu, Nepal (Accessed July 2014).
An Analytical Report on National Survey of Female Community Health Volunteers. Kathmandu, Nepal (Accessed July 2014).
14 BASICS II, the MOST Project, and USAID. Nepal Child Survival Case Study: Technical Report. Published by the Basic Support for Institutionalizing Child Survival Project (BASICS II) for the United States Agency for International Development. Arlington, Virginia, 2004.
15 USAID | DELIVER PROJECT, Task Order 4. 2014. Health Logistics in Nepal: Two Decades of Investments in Public Health Supply Chain Management: How Access to Supplies Improved Health Outcomes in Nepal. Arlington, Virginia. USAID | DELIVER PROJECT, Task Order 4.
16 Female Community Health Volunteer National Survey, 2014. Family Health Division, Department of Health Services, Ministry of Health and Population, Kathmandu, Nepal.
17 Creation UMesh. 2015. "Female Community Health Volunteer (FCHV) in Nepal." Accessed October 2015.
18 Department of Health Services, Ministry of Health and Population, Government of Nepal. 2012. Health Services Coverage: Fact Sheet. Kathmandu, Nepal: Ministry of Health and Population.
19 Dawson, P. 2012. Sharing Community-based Health Program Experiences: Nepal and Madagascar. Antananarivo, Madagascar: JSI Research & Training/MAHEFA.
20 Fiedler, J. 2000. "The Nepal National Vitamin A Program: prototype to emulate or donor enclave?" Health Policy and Planning 15, 2: 145-156.
Recommended Citation
Hannah Foehringer Merchant, Kristen Devlin and Kimberly Farnham Egan. 2016. Nepal's Community-based Health System Model: Structure, Strategies, and Learning. Arlington, VA: Advancing Partners & Communities.
